Measuring Real-World Sleep with Actigraphy: Three Clinical Trial Use Cases
Disturbed or impaired sleep has been the subject of increased research attention in recent years, as both a primary disorder and in cases where disturbed sleep is a symptom of another disease. Disturbed sleep is common in people with arthritis, atopic dermatitis, Alzheimer’s Disease, Parkinson’s Disease, and many other conditions. Research is focused on measuring and diagnosing these sleep disorders, as well as the development of new treatments to improve sleep across a broad range of indications. Wearable devices provide a low-burden and remote approach to objectively quantify people’s sleep in their real life, often revealing meaningful insights that might not be available with polysomnography or self-report data. While sleep architecture and sleep staging are difficult to estimate with accelerometry alone, actigraphy is sensitive to treatment effects in previous studies of sleep disorders.1
Use Case 1: Measuring Sleep in Rheumatoid Arthritis
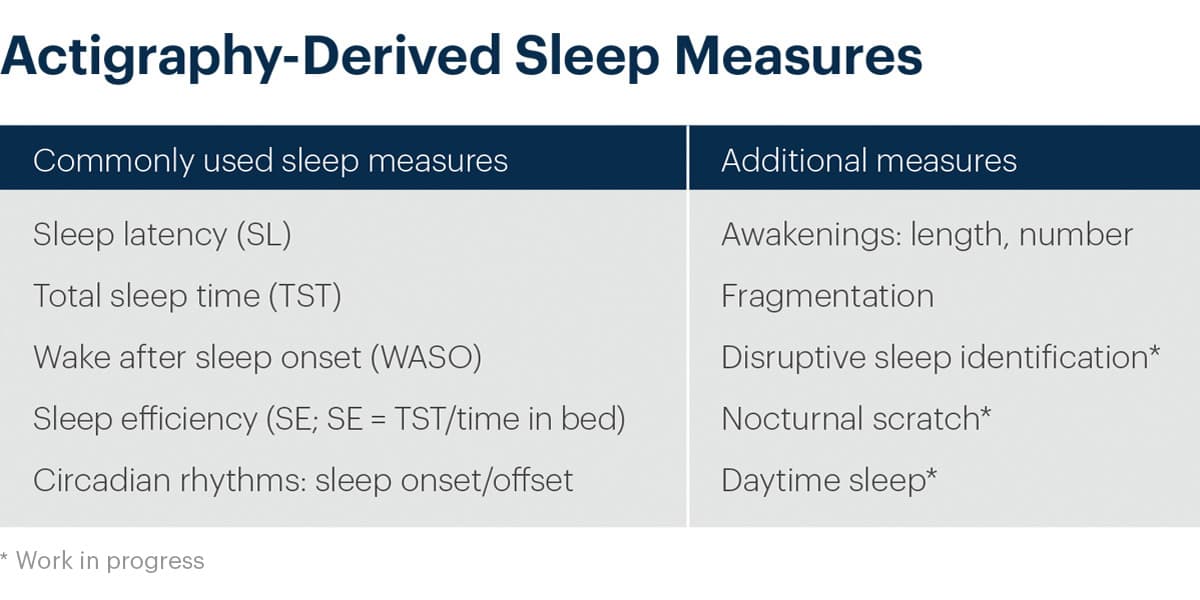
More than 80% of people with rheumatoid arthritis (RA) report fatigue as part of their symptoms.2 While most interventions are focused on reduction in pain, impaired sleep is an important indicator of disease severity and treatment effect. In studies with primary pain endpoints, actigraphy-derived sleep endpoints can help more fully characterize the participant’s experience. With continuous day and night wear periods, additional daily measures of physical activity can also be measured.
- In previous studies of rheumatoid arthritis, ActiGraph devices have shown high sensitivity and specificity for classification of sedentary time, light intensity, and moderate intensity physical activity.3
- In a current Phase 2 global RA trial, an ActiGraph CentrePoint Insight Watch is being used to measure total sleep time (TST), wake after sleep onset (WASO), and daily step counts as exploratory measures.
Use Case 2: Detecting Impaired Sleep in People with Neurodegenerative Diseases
Cognitive and functional decline are typical endpoints in neurodegenerative disorders. Sleep disturbances are the second most frequent non-motor complaints among people with Parkinson’s disease.4 Those with Alzheimer’s Disease have a higher prevalence of sleep disorders and behavioral disturbances than healthy elderly adults.5 Actigraphy has been shown to be an appropriate method to examine sleep disorders in dementia patients.6 Past studies have shown correlation between actigraphy measures can be valid predictors of tau pathology with potential clinical use.7
- Actigraphy-derived sleep measures detected significant treatment responses to a novel brain stimulation therapy in a recent PhI/II RCT study, corroborating improvements in Activity of Daily Living.8
- Walking speed and stride length have both been shown to be impacted in patients with dementia.9 With continuous day and night wear periods, additional measures of gait and walking speed can also be collected.
- In a recent Phase 2 global study of patients with dementia, researchers used an ActiGraph GT9X to track movement counts during sleep.
Use Case 3: Assessing Treatment Efficacy in Chronic Insomnia
One of the most common sleep disorders is insomnia, characterized by the recurring difficulty to fall or remain asleep despite motivation and means to do so. Most adults experience insomnia at some point of their lives, but when people exhibit symptoms at least three times per week for at least three months, insomnia is considered a chronic condition and clinical interventions might be necessary.
- The ActiGraph GT9X was used in a recent Ph2 study to assess the efficacy of medicinal cannabis on treating chronic insomnia.10 Actigraphy measures of total sleep time and sleep efficiency detected significant and substantial improvements associated with the treatment, corroborating self-reported sleep diary. On the other hand, polysomnography did not detect treatment effects, potentially due to the infrequency and laboratory setup of the assessments.
Compliance
Past studies have reported good compliance when using ActiGraph devices for collecting sleep measures in clinical trials. Participant compliance as high as 95% has been shown with wrist-worn device data collection wear periods.11 ActiGraph devices are easy to use, and every site and participant is trained on how to operate the device during a trial. CenterPoint, ActiGraph’s software ecosystem, allows for near real-time monitoring of compliance and wear periods.
End-to-End Data Transparency
ActiGraph’s fully transparent system relies on proven, open-source algorithms developed by the scientific community to generate meaningful, reliable measures. Full access to “future-proof” raw sensor data means that new and more sophisticated sleep algorithms and analysis techniques can be applied to collected data as they emerge. Trial sponsors are able maintain data comparability across phases and studies and derive the highest quality outcomes, now and in the future.
Experience
The ActiGraph platform has been used to measure sleep in dozens of indications across a broad range of therapeutic areas. ActiGraph devices have been used to measure sleep endpoints in more than 50 Phase 2 and Phase 3 industry-sponsored clinical trials since 2015.
Are you interested in learning more about how actigraphy-derived sleep measures can enhance your clinical development program? Contact us to speak with a member of our team.
References:
- Zeitzer, Jamie M et al. “Effect of Suvorexant vs Placebo on Total Daytime Sleep Hours in Shift Workers: A Randomized Clinical Trial.” JAMA network open vol. 3,6 e206614. 1 Jun. 2020, doi:10.1001/jamanetworkopen.2020.6614
- Arthritis Foundation. https://www.arthritis.org
- O’Brien, Ciara M et al. “Measurement of sedentary time and physical activity in rheumatoid arthritis: an ActiGraph and activPALtmvalidation study.” Rheumatology international vol. 40,9 (2020): 1509-1518. doi:10.1007/s00296-020- 04608-2
- Loddo, Giuseppe et al.“The Treatment of Sleep Disorders in Parkinson’s Disease: From Research to Clinical Practice.” Frontiers in neurology vol. 8 42. 16 Feb. 2017, doi:10.3389/fneur.2017.00042
- Zhou, Guoyu MD, PhD; Liu, Shuangwu MD; Yu, Xiaolin MD; Zhao, Xinjin MD; Ma, Lin MD; Shan, Peiyan MD, High prevalence of sleep disorders and behavioral and psychological symptoms of dementia in late-onset Alzheimer disease, Medicine: December 2019 – Volume 98 – Issue 50 – p e18405
- Brzecka, Anna et al. “Sleep Disorders Associated With Alzheimer’s Disease: A Perspective.” Frontiers in neuroscience vol. 12 330. 31 May. 2018, doi:10.3389/fnins.2018.00330
- López-García, Sara et al. “Sleep Time Estimated by an Actigraphy Watch Correlates With CSF Tau in Cognitively Unimpaired Elders: The Modulatory Role of APOE.” Frontiers in aging neuroscience vol. 13 663446. 2 Aug. 2021, doi:10.3389/fnagi.2021.663446
- Cimenser, A. et al. Sensory-Evoked 40-Hz Gamma Oscillation Improves Sleep and Daily Living Activities in Alzheimer’s Disease Patients. Front. Syst. Neurosci. 15, 746859 (2021).
- Beauchet, Olivier et al. “Gait analysis in demented subjects: Interests and perspectives.” Neuropsychiatric disease and treatment vol. 4,1 (2008): 155-60. doi:10.2147/ndt.s2070
- Jennifer H Walsh, Kathleen J Maddison, Tim Rankin, Kevin Murray, Nigel McArdle, Melissa J Ree, David R Hillman, Peter R Eastwood, Treating insomnia symptoms with medicinal cannabis: a randomized, crossover trial of the efficacy of a cannabinoid medicine compared with placebo, Sleep, Volume 44, Issue 11, November 2021, zsab149, https://doi.org/10.1093/sleep/zsab149
- Melby, Katrine et al. “Actigraphy assessment of motor activity and sleep in patients with alcohol withdrawal syndrome and the effects of intranasal oxytocin.” PloS one vol. 15,2 e0228700. 13 Feb. 2020, doi:10.1371/journal. pone.0228700