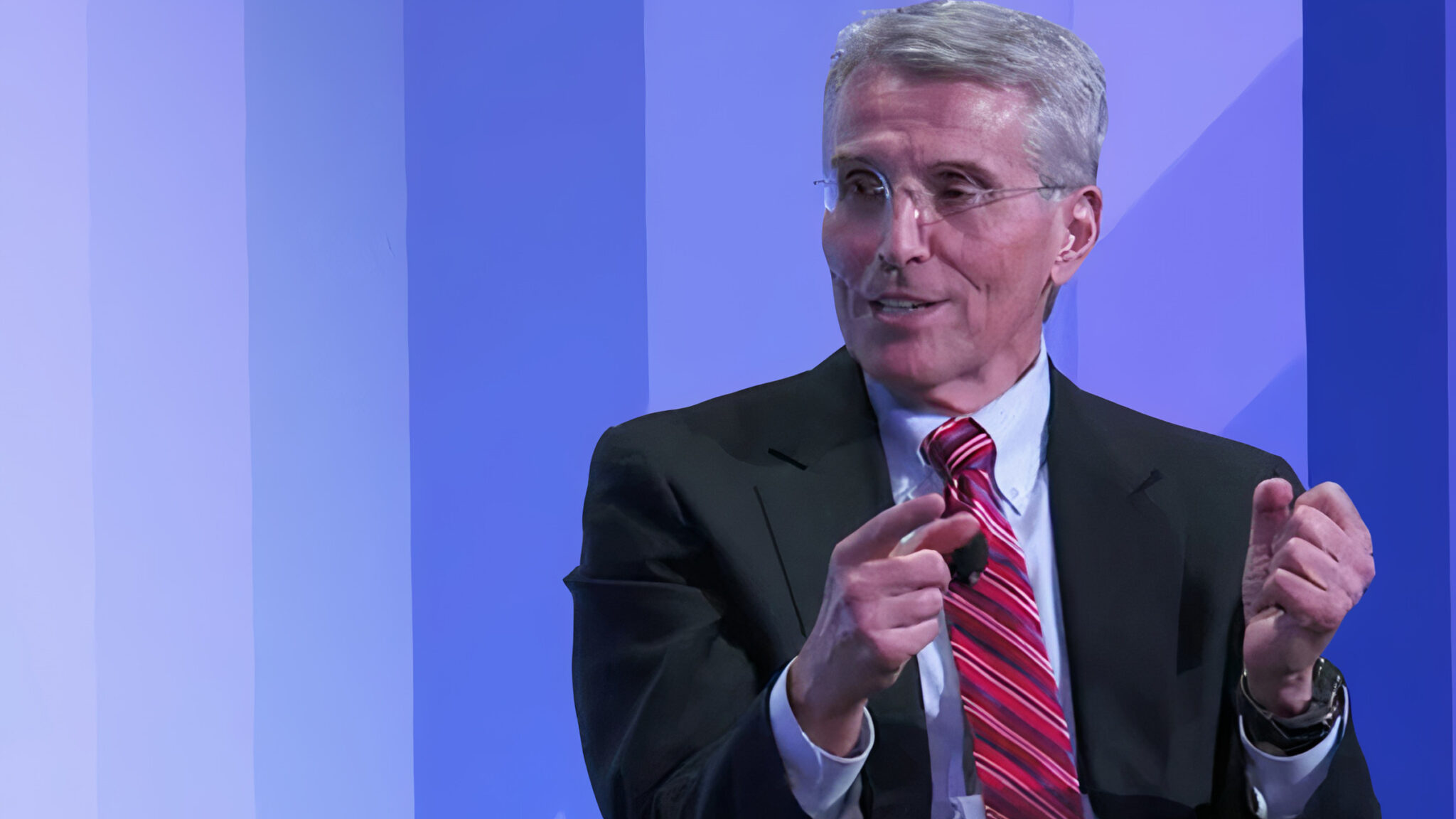
Richard Pazdur, FDA's OCE director (Flatiron Health via YouTube)
FDA's OCE makes the case for accelerated approval rider in user fee reauthorization
Four experts from the FDA’s Oncology Center of Excellence took to the New England Journal of Medicine yesterday to make the case for not only …
Sign up to read this article for free.
Get free access to a limited number of articles, plus choose newsletters to get straight to your inbox.