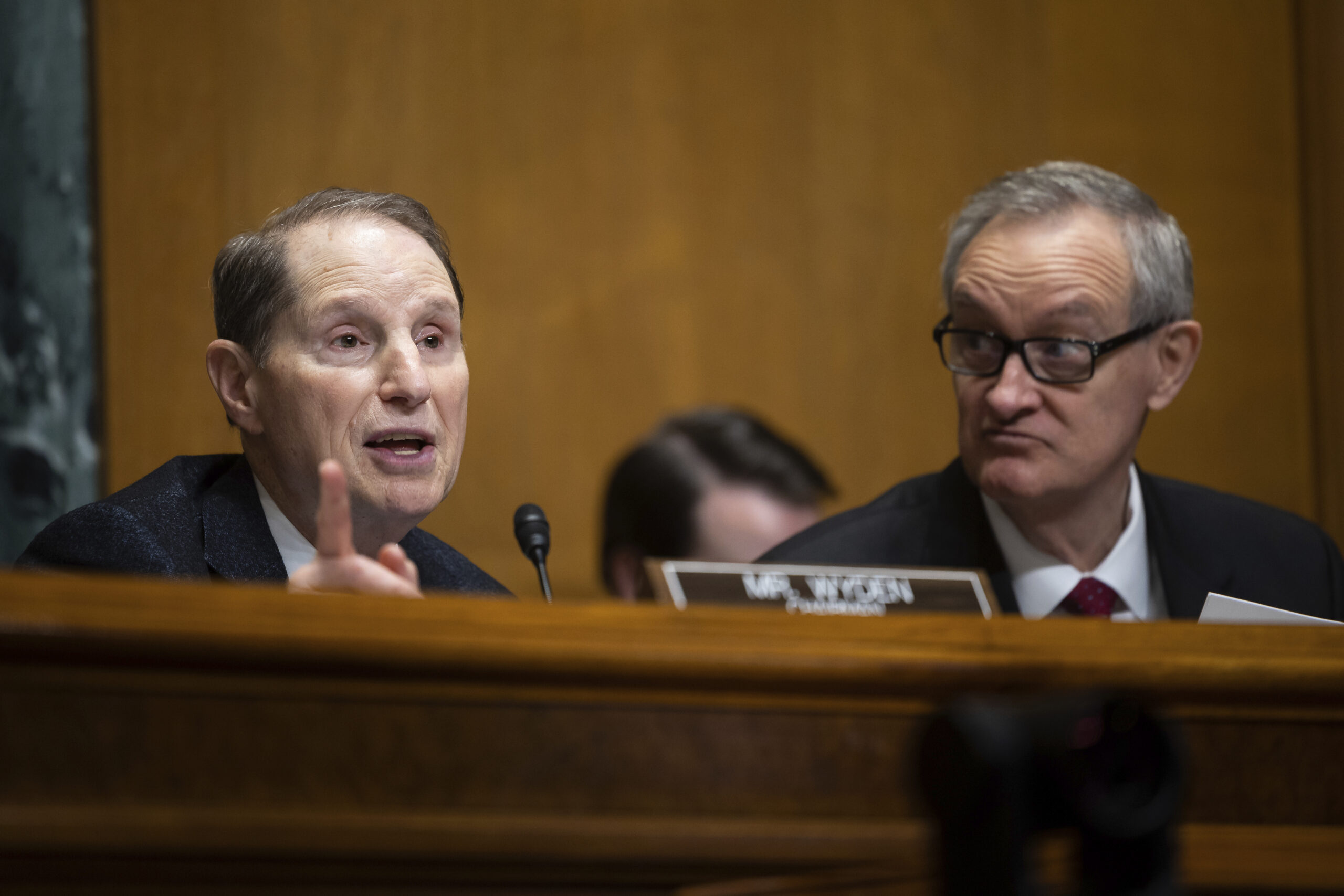
Sens. Ron Wyden (D-OR) and Mike Crapo (R-ID) (Francis Chung/Politico via AP Images)
PBM reforms: Senate Finance Committee leaders introduce another bipartisan bill
Last summer’s bipartisan, bicameral focus on the pharma middlemen known as pharmacy benefit managers is returning. Sens. Ron Wyden (D-OR) and Mike Crapo (R-ID) introduced …
Sign up to read this article for free.
Get free access to a limited number of articles, plus choose newsletters to get straight to your inbox.