Minimal Residual Disease: A Prognostic Factor Moving the Needle in Patient Care
As technology advances, innovative diagnostic tools that may help guide therapeutic decision-making are becoming available to more and more healthcare professionals (HCPs).
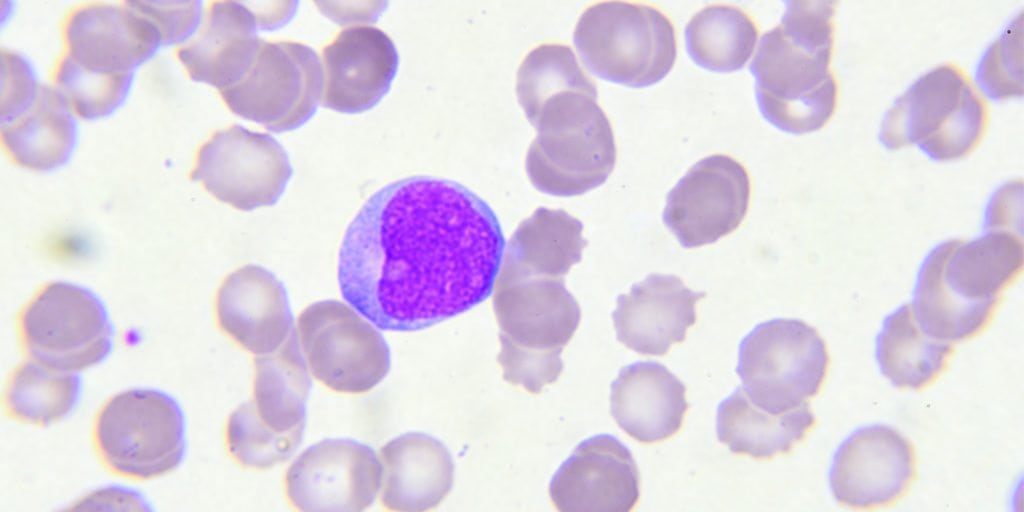
In the past, blood cancers like acute lymphoblastic leukemia (ALL) were primarily evaluated under a microscope to detect remaining cancerous cells during and after treatment. Now, there are more precise tools to identify minute amounts of cancer, known as measurable or minimal residual disease (MRD), present at concentrations that less sensitive tests, such as microscopy, could not detect.1
Tests for MRD have shown to better assess drug response and relapse risk than standard techniques, the results of which will equip HCPs with more accurate information about which patients may require further intervention and which can be spared additional therapy.1
“Over the last 20 years we have made significant advancements not only in the science of MRD detection, but in its potential impact as it relates to treatment of patients living with certain blood cancers,” said David M. Reese, M.D., senior vice president, Translational Sciences and Oncology, Amgen.
“The technology has advanced to the point where we definitely need to redefine what our goals of therapy are, and for every patient with a blood cancer we should be striving to achieve an MRD negative remission,” said Aaron Logan, M.D., PhD. hematologist.
MRD is usually evaluated in one of two ways. The first, called flow cytometry, uses cell-surface protein markers to differentiate between cells that are normal and those that are cancerous.2MRD can also be tested through DNA-based methods that can identify genetic alterations and over-expressed genes responsible for causing cancer.2
Compared to conventional testing methods that detect cancer cells in the bone marrow or blood with a sensitivity of about 1 in 20, these MRD testing methods have improved detection to sensitivities of 1 in 10,000 cells or better.2,3
Regardless of the method used to measure MRD, a negative status has been shown to correlate with improved clinical outcomes.4According to Dr. Logan, MRD status is “an extremely important prognostic factor for predicting whether a patient is likely to relapse after achieving remission.”
Because MRD is a quantification of disease burden, it can also be leveraged at several points in time, not just after the achievement of remission.1,4
“There’s a growing interest in using MRD not only for risk stratifying patients and to predict their outcomes, but also to identify strategies for intervening upon residual disease,” said Dr. Logan.
When used during treatment, MRD levels can indicate a patient’s response to therapy, as Dr. Logan explains.1Despite the impact MRD can play on risk stratification for patients, Dr. Logan notes not all labs are able to detect MRD at levels sensitive enough to understand the true impact.
However, he adds, “awareness of the importance of MRD is increasing. I do think more and more providers who see ALL patients are going to be finding ways to conduct MRD assessments on their patients.”
Beyond ALL, MRD testing has been used across a variety of hematologic malignancies, including other types of leukemia, certain lymphomas, and multiple myeloma.5Clinical research continues to explore the significance of MRD in these cancers.
“We still have a ton of work to do to,” Dr. Logan explains, “to investigate in all of these blood cancers what is the threshold at which we should change therapy, what are the most effective therapies and then once you achieve an MRD-negative remission, what do you do then to maintain that remission?”
Ultimately, Dr. Logan believes that the field is heading in a direction that will lead to better decision making.
Outside of the lab, the path appears to be moving quickly. According to a 2017 analysis by the U.S. Food and Drug Administration, nearly 40 percent of new drug and biologics license applications submitted to the Division of Hematology Products between 2014 and 2016 included MRD data.6
“At Amgen, we have been able to take what we are seeing in the lab after examining residual cancer cells and apply these learnings to our clinical development programs,” said Reese. “As testing for MRD continues to advance and becomes more commercially available, there is every expectation that treatment approaches will evolve to help better care for these patients.”
For more information on MRD and other advancements in oncology, please visit www.AmgenOncology.com.
References:
- Paeitta E. Bone Marrow Transplant. 2002;29:459-465.
- Brüggemann M, et al. Blood. 2012;120:4470-4481.
- Gökbuget N, et al. Blood. 2012;120:1868-1876.
- Berry D, et al. JAMA Oncol. 2017; 3:e170580.
- van der Velden VH, et al. Leukemia. 2003;17:1013-1034.
- Gormley N, et al. J Clin Oncol.2017;35:(suppl; abstr 2541)
USA-103-80026