The Rare Kidney Disease Playbook: How New Research and Innovation is Transforming the RKD Treatment Landscape
As kidney professionals from around the world converge at ASN’s Kidney Week 2023, Travere Therapeutics’ Eric Dube, Chief Executive Officer, Jula Inrig, Chief Medical Officer, and Peter Heerma, Chief Commercial Officer share their perspectives on how innovation in rare kidney disease (RKD) is transforming the treatment landscape.
How has the R&D landscape in rare kidney disease (RKD) changed?
 Jula Inrig,
Jula Inrig,Chief Medical Officer
Inrig: “For decades, very few clinical trials were conducted in chronic kidney disease, and almost none in RKDs like IgA nephropathy (IgAN). A key factor limiting early research was using kidney failure or death as endpoints, which made clinical trials for new therapies prohibitively long and costly to conduct, and trial recruitment incredibly challenging. In 2012, the Kidney Health Initiative (KHI), a public-private partnership comprised of the American Society of Nephrology (ASN), the US Food and Drug Administration (FDA), and numerous biopharma companies, academic researchers, and patient advocacy organizations, came together determined to advance the nephrology field and accelerate RKD research. We identified proteinuria (high levels of protein in the urine that indicate damage to the filters in the kidney), which means the kidneys are no longer filtering properly, as a potential new surrogate endpoint. Proteinuria reduction and remission of proteinuria were already key measures of kidney function and regularly used in clinical practice all over the world. Testing for proteinuria is simple and non-invasive, making it an ideal way to measure risk of kidney disease progression. Today, there are over 30 ongoing trials in IgAN. As a nephrologist, it’s exciting to see the advancements in research and that these patients now have new treatment options for their condition – which wasn’t the case for so many years. It’s also exciting to see the potential these medicines have of being combined and working together to help delay the progression to kidney failure. As a physician, every year that you can keep a patient from dialysis or a kidney transplant, is a year with a higher quality of life… it’s a year that can be spent earning a degree, growing a career, or starting a family free from that burden. That’s gratifying, and a testament to the power of public-private partnerships and the innovation that companies like Travere are bringing to the field.”
Before we dig deeper into surrogate endpoints in RKD and IgAN. For those who may not be familiar with Travere or IgAN, can you tell us a little more about the company and the condition?
 Eric Dube,
Eric Dube,Chief Executive Officer
Dube: “Travere Therapeutics is biopharmaceutical company based out of San Diego. We’re proud to be in rare for life. We are advancing a pipeline of potential first-in-class medicines targeting rare diseases with significant unmet needs. Many of the people who work at Travere are rare disease patients, survivors, and caregivers themselves and we’re fortunate to have many passionate colleagues, like Jula, who have been a driving force in delivering innovation in RKD for years. Keeping patients’ interests top of mind is at the heart of our mission and drives our commitment to meeting the unique needs of the rare patient communities we serve. It’s why Travere has actively tried to raise the bar in our research of RKD by designing trials using an active control that is a standard of care instead of placebo — some of the most robust and rigorous pivotal trials in the category.”
 Peter Heerma,
Peter Heerma,Chief Commercial Officer
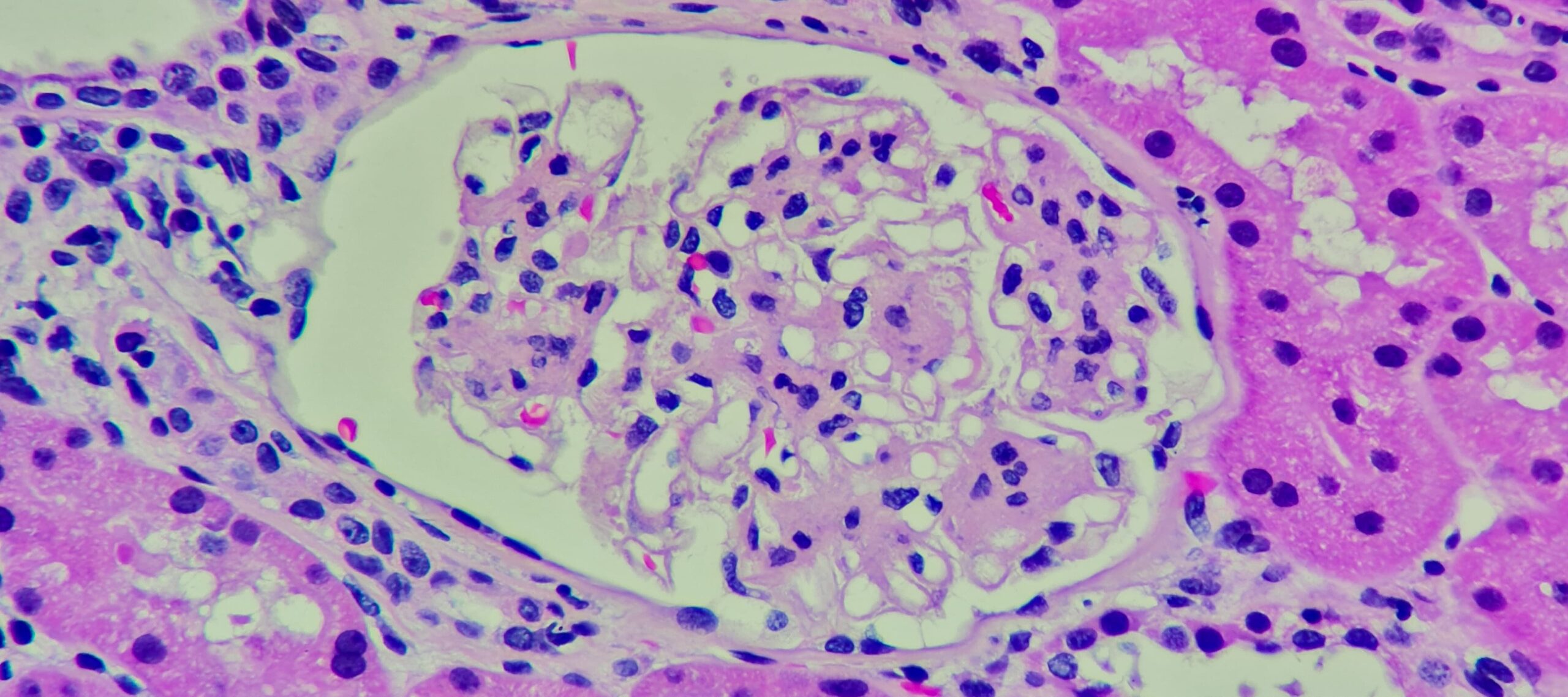
Heerma: “Also called Berger’s disease, IgAN damages the small blood vessels that filter waste in your kidneys. While classified as rare – affecting approximately 150,000 in the United States – IgAN is one of the most common and more rapidly progressing kidney diseases leading to kidney failure. The disease typically develops in people who are in their 20s or 30s – who are in the prime of their lives, and then suddenly feel fatigue, pain, experience swelling in their hands or feet, and don’t know what’s happening to them. Many patients face a long journey to diagnosis, and more than two-thirds of patients are at an advanced stage of the disease once diagnosed. A high proportion of individuals diagnosed with IgAN do not sufficiently respond to the historical standard of care treatment, which often includes hypertension drugs such as angiotensin receptor blockers (ARBs), angiotensin-converting enzyme (ACE) inhibitors, and steroids. As a result, many will struggle to manage their disease and progress more quickly to kidney failure.”
How has using proteinuria as a surrogate endpoint in clinical trials spurred innovation in IgA nephropathy?
Inrig: “KHI identified proteinuria as a reliable predictor of a treatment’s effect on long-term kidney outcomes, and research continues to show evidence of the connection between proteinuria and kidney failure. A recent groundbreaking analysis of the UK National Registry of Rare Kidney Diseases (RaDaR) showed that patients that have been traditionally regarded as ‘low risk’ (with proteinuria <1 g/day) can still progress to kidney failure within 10-15 years. The RaDaR findings can be practice-changing because historically patients and physicians did not realize just how aggressive IgAN is, and how much damage it can do in a relatively short period of time. While that finding was sobering, the study also revealed some good news – the decline in kidney function can be slowed, with data showing that a 50% reduction in proteinuria can delay time to kidney failure or death by 8.5 years. For a patient facing kidney failure and potentially dialysis, every day counts.”
Heerma: “We regularly speak with patients who share not only the physical, but the overwhelming psychological, social, and financial challenges that can be part of living with RKD. These are individuals who considered themselves healthy and then very quickly find themselves putting their lives on hold to prepare for dialysis or transplant. Dialysis is burdensome for these patients, often requiring at least 9 hours or more per week connected to a machine that helps to partially replace your kidney function by cleaning and filtering your blood. RaDaR demonstrated the connection between increased proteinuria levels and declining kidney function is indisputable and has created a new urgency to treat IgAN patients earlier and more aggressively to prevent rapid disease progression.”
What inspires you to be in rare disease?
Dube: “I often say I’m ‘impatient for patients.’ My decision to work in the life sciences industry was reinforced when I was diagnosed with two rare cancers. That gave me a new perspective on the importance of time. I am certain our industry can provide that time and change people’s lives. After my own experience, I was also motivated to do my part in ensuring no family has to hear ‘there’s no effective therapy for your rare condition.’ Working in rare disease, there’s a true sense of community and a shared feeling that we are stronger together – and in this together. A step forward is progress for the entire community.”
Inrig: “Developing effective therapies is about improving quality of life as much as it is adding years to a life. I chose to go into nephrology because it was an under-researched area – the need, combined with the complex problems the field presents and the ability to develop relationships with patients while working with them over long periods of time, made the choice obvious for me. One of my former patients started dialysis when she was 17 years old and lived transfusion-to-transfusion until she passed away. She served as a member of a Patient and Family Council that advised the KHI and helped usher in a new era of trial design. Not a week goes by that I don’t think about her – and what she might have accomplished, given the opportunity.”