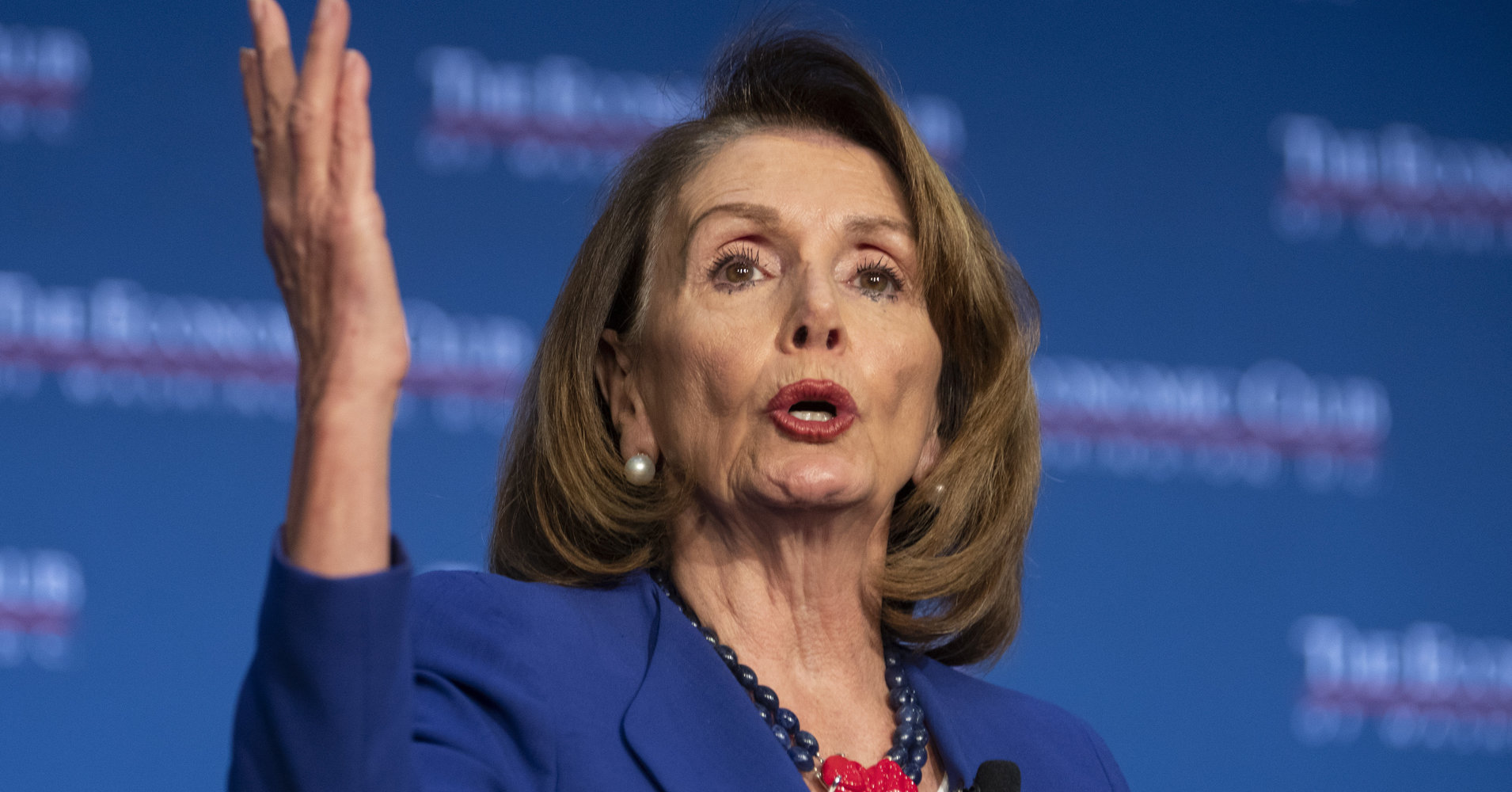
Speaker Nancy Pelosi to unveil bill for federally negotiated drug prices
After months of buzz from both sides of the aisle, Speaker Nancy Pelosi will today introduce her plan to allow the federal government to negotiate prices for 250 prescription drugs, setting up a showdown with a pharmaceutical industry working overtime to prevent it.
The need to limit drug prices is a rare point of agreement between President Trump and Democrats, although the president has yet to comment on the proposal and will likely face pressure to back a more conservative option or no bill at all. Republican Senator Chuck Grassley is reportedly lobbying his fellow party members on a more modest proposal he negotiated with Democratic Senator Ron Wyden in July.
Unlock this article instantly by becoming a free subscriber.
You’ll get access to free articles each month, plus you can customize what newsletters get delivered to your inbox each week, including breaking news.