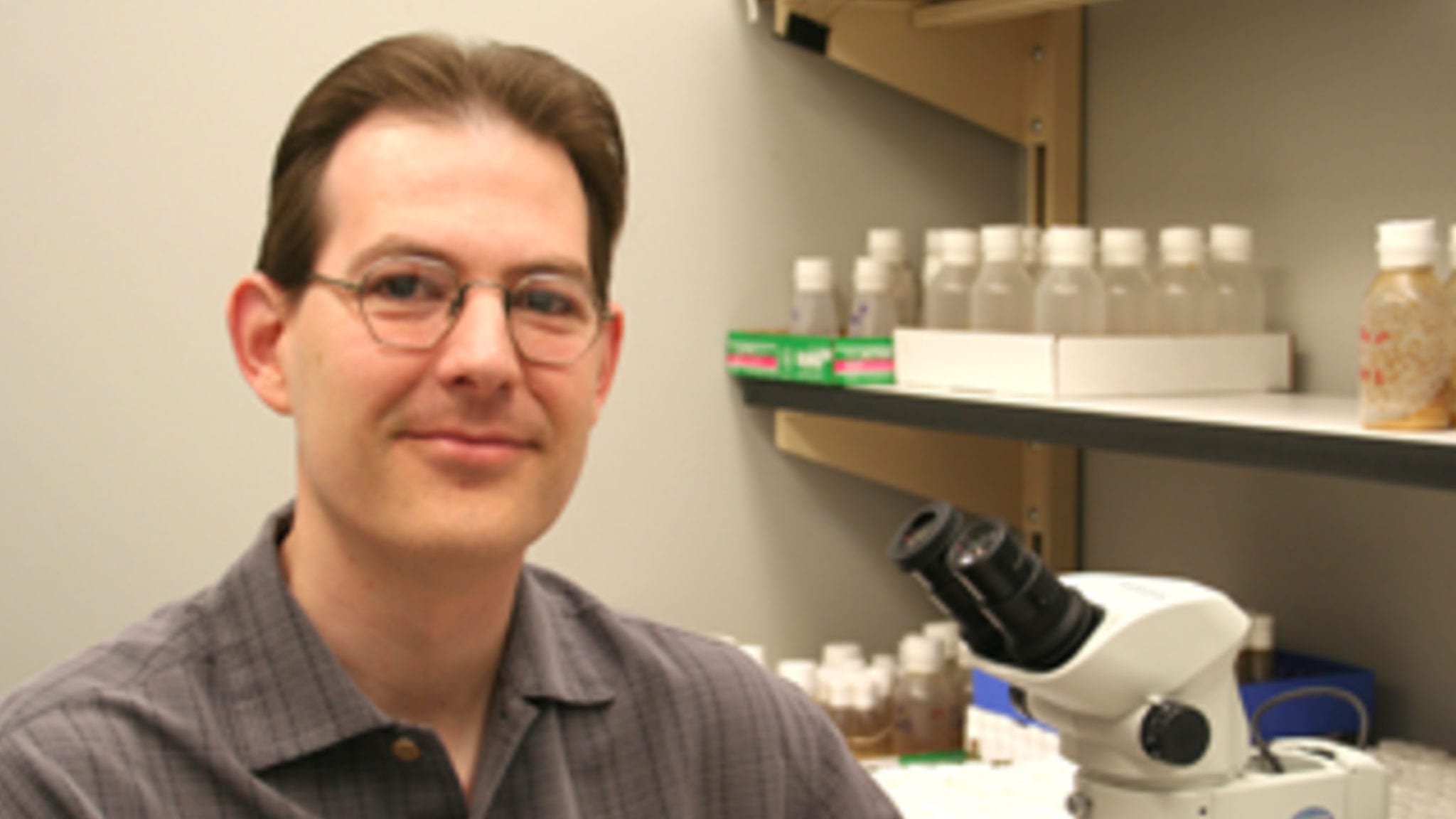
Charles Nichols, LSU School of Medicine
Could psychedelics tackle the obesity crisis? A longtime researcher in the field says his latest mouse study suggests potential
Psychedelics have experienced a renaissance in recent years amid a torrent of preclinical and clinical research suggesting it might provide a path to …
Sign up to read this article for free.
Get free access to a limited number of articles, plus choose newsletters to get straight to your inbox.